Understanding the differences between type 1 and type 2 diabetes is essential for anyone navigating the complexities of these chronic conditions. Both forms can affect how your body uses insulin, but their causes, symptoms, and management strategies vary significantly. In this article, we’ll break down what sets them apart and clarify common misconceptions.
Whether you’re newly diagnosed, supporting a loved one, or simply looking to expand your knowledge, this guide offers insights that can empower you. Join us as we delve into the fundamental differences between type 1 and type 2 diabetes, ensuring you’re well-informed on this critical health topic.

Understanding Type 1 and Type 2 Diabetes
Diabetes is a chronic medical condition that affects how your body processes blood sugar (glucose). Type 1 and Type 2 diabetes are the two primary forms of this illness. Understanding the differences between them is critical to proper management and treatment. Type 1 diabetes usually develops in children and young adults, making it an autoimmune condition where the body attacks insulin-producing cells in the pancreas. Consequently, people with Type 1 diabetes need to take insulin daily to manage their blood sugar levels.
Type 2 diabetes, on the other hand, is more common and can develop at any age, typically in adults. In this condition, the body either becomes resistant to insulin or doesn’t produce enough to maintain normal glucose levels. Lifestyle factors, including diet and exercise, play a significant role in its development and management. Understanding these basics will help in recognizing the significance of lifestyle choices in controlling diabetes.
To learn about your risk factors, consider using the app mySugr. This application offers personalized insights into your diabetes management and allows you to track blood sugar levels, carb intake, and medication schedules. Download it from your smartphone’s app store for more personalized guidance.
Moreover, discussions with healthcare professionals are crucial. They can provide tailored education about diabetes based on your health situation. Websites like the American Diabetes Association (ADA) can also offer extensive resources about both types of diabetes, including articles and toolkits aimed at helping individuals understand their condition thoroughly.
Understanding diabetes empowers individuals to take control of their health, leading to improved management strategies and better overall outcomes. With continuous education, people living with diabetes can lead active, fulfilling lives.
Common Symptoms of Type 1 and Type 2 Diabetes
Recognizing the symptoms of diabetes is vital for early intervention and successful management. The primary symptoms common to both Type 1 and Type 2 diabetes include excessive thirst, frequent urination, extreme hunger, fatigue, and blurred vision. These symptoms occur because high blood sugar levels can cause the body to lose fluids rapidly, leading to dehydration.
In Type 1 diabetes, symptoms may develop suddenly and be severe. Young people especially may present symptoms such as rapid weight loss and irritability. If a child or adolescent shows these signs, immediate medical consultation is necessary. Using a symptom checker app such as Diabetes:M can help track these symptoms effectively. This app helps users log their symptoms and glucose levels, providing meaningful insights into their condition.
For Type 2 diabetes, symptoms can develop more gradually, making them easier to overlook. People may also experience numbness or tingling in the hands or feet, poor wound healing, and skin infections. If you notice any combination of these symptoms, it is essential to schedule a check-up with a healthcare provider, as they can discuss potential testing and diagnosis.
Informational websites like Diabetes.co.uk offer an overview of these symptoms and allow users to take quizzes that assess their risk of diabetes. Engaging with these resources can provide better awareness and understanding of what to look for in terms of symptoms.
Left untreated, both forms of diabetes can lead to serious health complications. Recognizing and addressing symptoms early is key to managing the condition and maintaining a good quality of life. By utilizing apps and trusted health resources, individuals can stay informed and proactive about their health.
How to Manage Type 1 and Type 2 Diabetes Effectively
Managing diabetes effectively involves a combination of medication, dietary choices, and lifestyle changes. For individuals with Type 1 diabetes, insulin therapy is necessary. It is critical to work with a healthcare provider to create a personalized insulin regimen that may include different types of insulin that work at various speeds. Tracking your insulin doses can be efficiently done using apps like My Diabetes Home, which allow you to monitor both insulin and glucose levels.
For Type 2 diabetes, lifestyle management is essential. It begins with asking the right questions about diet. Integrating foods that have a low glycemic index can help manage blood sugar levels. Meal planning tools available on the app Lose It! offer useful guidance for making healthier food choices. Users can set weight goals and track their calorie intake effectively through this app.
Regular physical activity is another cornerstone of effective diabetes management. The CDC suggests at least 150 minutes of moderate-intensity aerobic activity weekly for adults. Using fitness-tracking apps like Fitbit can assist in maintaining an active lifestyle by setting step goals and tracking workouts.
Educational resources are also invaluable in managing diabetes. Online platforms such as Diabetes.org provide webinars, newsletters, and community support groups that can offer emotional support and practical advice on living with diabetes. Sharing experiences with others can encourage positive lifestyle adjustments.
Lastly, routine checkups with healthcare professionals are vital. Regular screenings for complications, as well as consistent monitoring of blood sugar levels, can help in achieving optimal diabetes management. Engaging with apps that remind you of appointments, like Plump, can also help keep track of your health journey.
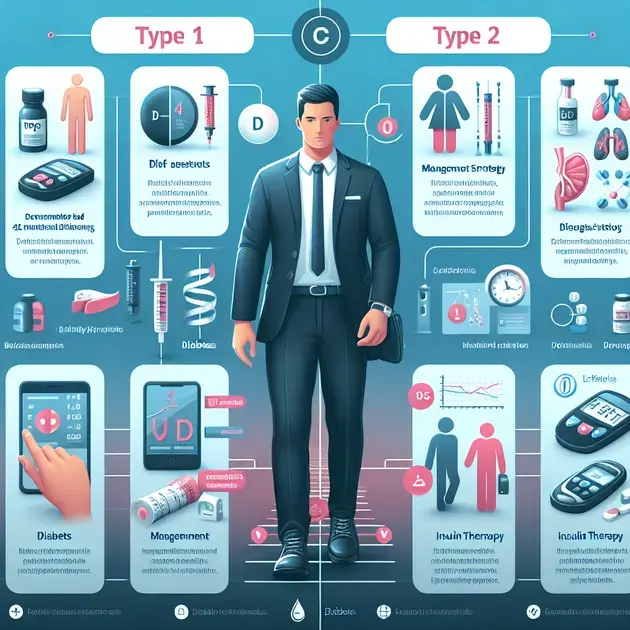
Understanding Type 1 Diabetes and Type 2 Diabetes
Diabetes is a complex health condition that affects millions of people worldwide. When we talk about diabetes, we generally refer to two main types: type 1 diabetes and type 2 diabetes. Understanding the differences between these two types is crucial for effective management and treatment. Type 1 diabetes is an autoimmune condition, where the body’s immune system mistakenly attacks insulin-producing cells in the pancreas. This type usually appears during childhood or adolescence, but it can occur in adults as well.
On the other hand, type 2 diabetes is more common and typically develops in adults, although it increasingly affects younger populations due to lifestyle factors. In this condition, the body either becomes resistant to insulin or doesn’t produce enough to maintain normal glucose levels. This results in elevated blood sugar levels, which can lead to various health complications if left untreated.
Moreover, managing type 1 diabetes often involves a regimen of insulin therapy, whereas type 2 diabetes can often be managed with lifestyle changes, oral medications, and sometimes insulin. Recognizing the relationship and differences between these two types can greatly influence treatment choices and health outcomes.
In this space, it’s vital to highlight that individuals with type 1 diabetes depend on insulin for survival, whereas those with type 2 diabetes may find success in managing their condition through diet, exercise, and monitoring blood sugar levels. Knowing the nuances can empower patients to take charge of their health more effectively.
In summary, comprehending the distinctions and similarities between type 1 diabetes and type 2 diabetes is essential for anyone looking to gain better control over their health or support someone who is affected by these conditions.
Symptoms of Type 1 Diabetes and Type 2 Diabetes
Symptoms can vary between type 1 diabetes and type 2 diabetes, but many overlap. It’s important to recognize these symptoms early for timely diagnosis and management. In type 1 diabetes, symptoms often appear suddenly and can include excessive thirst, frequent urination, and unexplained weight loss. Children and teenagers are particularly vulnerable to these symptoms.
Type 2 diabetes symptoms tend to develop more gradually. Individuals may experience increased thirst and hunger, frequent urination, fatigue, and blurred vision. However, some people may not show symptoms at all, making regular screening essential for early detection and intervention.
Another aspect of symptoms is the occurrence of diabetic ketoacidosis (DKA), primarily associated with type 1 diabetes. This serious condition occurs when the body starts breaking down fat at an alarming rate, leading to the buildup of ketones, which can cause severe health issues. Recognizing the early signs of DKA is critical and can save lives.
In contrast, while type 2 diabetes can lead to hyperglycemic crises, it is less commonly linked to life-threatening conditions like DKA. However, uncontrolled type 2 diabetes poses significant long-term health risks like cardiovascular disease and kidney damage.
Being aware of the signs and symptoms of both type 1 diabetes and type 2 diabetes can alert individuals to seek medical advice sooner rather than later, potentially preventing or mitigating severe complications.
Diagnosis of Type 1 Diabetes and Type 2 Diabetes
Diagnosing diabetes is crucial for effective management and treatment. Healthcare providers typically use several methods to diagnose both type 1 diabetes and type 2 diabetes. The most common diagnostic tests include fasting blood glucose tests, the oral glucose tolerance test, and hemoglobin A1c testing.
The fasting blood glucose test measures blood sugar levels after an overnight fast. If the levels are greater than 126 mg/dL, diabetes is suspected. The oral glucose tolerance test involves fasting overnight, then consuming a sugary drink, with blood samples taken afterward to monitor how the body processes sugar.
Hemoglobin A1c testing provides a snapshot of average blood glucose levels over the past two to three months. An A1c level of 6.5% or higher indicates diabetes. It’s crucial to understand that while these tests are effective, the diagnosis should involve a comprehensive evaluation by a healthcare professional to determine whether the diabetes is of type 1 or type 2.
In some cases, additional tests may be required, especially in ambiguous situations. Autoantibody tests can help distinguish type 1 from type 2 diabetes. Typically, those with type 1 will exhibit specific autoantibodies that indicate an autoimmune response against insulin-producing cells.
Early and accurate diagnosis of diabetes is imperative as it influences treatment plans and potential lifestyle modifications necessary for managing blood sugar levels effectively.
Management Strategies for Type 1 Diabetes and Type 2 Diabetes
Managing diabetes effectively requires a multifaceted approach tailored to each individual’s type and needs. For individuals with type 1 diabetes, the primary management strategy is insulin therapy. This involves monitoring blood sugar levels closely and administering the correct amount of insulin before meals based on carbohydrate intake.
In contrast, management strategies for type 2 diabetes often emphasize lifestyle modifications, including diet and exercise. A balanced diet low in refined sugars and rich in whole foods can help manage blood glucose levels effectively. Regular physical activity not only aids in weight management but also improves the body’s insulin sensitivity, making type 2 diabetes more manageable.
Medication may also come into play for those with type 2 diabetes. There are various oral medications available that work in different ways to lower blood sugar levels. For some individuals, insulin may be necessary as the disease progresses. Collaboration with healthcare providers is essential to determine the most effective treatment regimen.
In addition to medication and lifestyle changes, regular monitoring of blood sugar levels is crucial for all individuals with diabetes. This can provide real-time insights into how food, exercise, and other factors impact glucose levels, allowing for timely interventions when necessary.
Education and support play significant roles in effective management as well. Understanding the condition, its implications, and how to recognize warning signs can empower individuals to make informed choices and adhere to their management plans more consistently.
Complications Associated with Type 1 Diabetes and Type 2 Diabetes
Both type 1 diabetes and type 2 diabetes carry the risk of various complications if not managed properly. Understanding these potential health issues is crucial for preventing them. One of the major complications associated with diabetes is cardiovascular disease. High blood sugar levels can damage blood vessels and nerves, leading to serious heart problems.
Another common complication is neuropathy, which affects the nerves. Diabetic neuropathy can lead to numbness and pain in the extremities. Furthermore, individuals with diabetes are at an increased risk for foot problems, which can escalate to serious infections requiring amputation if not managed correctly.
Kidney damage, or nephropathy, is another severe complication associated mainly with diabetes. The kidneys filter waste from the blood, and prolonged exposure to high blood sugar can affect their function, leading to kidney disease or failure over time.
Moreover, complications such as retinopathy can lead to vision problems, even blindness. High blood sugar levels can damage the blood vessels in the retina, leading to significant vision loss if left untreated. Routine eye checks are essential for early detection and treatment.
Lastly, both types of diabetes can lead to skin conditions, infections, and complications during pregnancy, emphasizing the need for tight glucose control and frequent check-ups with healthcare providers. Awareness of these complications can encourage individuals to maintain their health diligently, minimizing risks associated with diabetes.
Conclusion
Understanding the key differences between Type 1 and Type 2 diabetes is essential for effective management and treatment of these chronic conditions. Type 1 diabetes is often diagnosed in the younger population and requires lifelong insulin therapy as the immune system attacks insulin-producing cells. In contrast, Type 2 diabetes typically occurs in adults and can often be managed through lifestyle changes, dietary adjustments, and, if necessary, medication. Recognizing this distinction allows individuals to better navigate their health journeys and make informed decisions.
It is crucial to be aware of the common symptoms associated with both types of diabetes. Early detection and timely intervention can significantly reduce the risk of serious complications such as cardiovascular disease, neuropathy, and kidney damage. Using technology, such as diabetes management apps and symptom trackers, can greatly aid in monitoring blood sugar levels and maintaining a healthy lifestyle. Moreover, open discussions with healthcare professionals can provide tailored guidance and support, fostering a proactive approach to diabetes management.
In addition to the medical aspects, continuous education and community support can empower individuals living with diabetes. Engaging with educational resources, attending workshops, and participating in support groups can enhance one’s understanding and capability to manage the condition effectively. Ultimately, by prioritizing health, recognizing symptoms early, and utilizing both medical and communal resources, individuals can lead healthier, fulfilling lives while navigating their diabetes journey.
