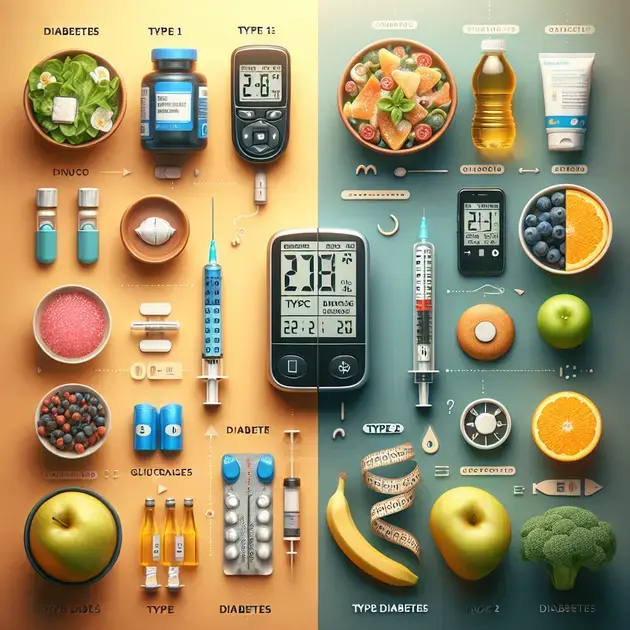
Understanding the difference between type 1 and type 2 diabetes is crucial for effective management and care. While both conditions impact blood sugar regulation, their causes, symptoms, and treatment approaches significantly differ. In this article, we’ll break down these differences, empowering you with the knowledge needed to distinguish between these two diabetes types and make informed health decisions.
Whether you’re navigating a recent diagnosis or are simply curious about diabetes, gaining clarity on type 1 and type 2 can lead to better health outcomes. Join us as we delve into their unique characteristics, enabling a deeper understanding of each condition.

Understanding Type 1 Diabetes
Type 1 diabetes is a chronic condition where the pancreas produces little or no insulin. This form of diabetes is often diagnosed in children and young adults, hence its previous name, juvenile diabetes. Understanding the underlying mechanisms of Type 1 diabetes is vital for effective management and healthcare. Unlike Type 2 diabetes, which is often associated with lifestyle factors, Type 1 is an autoimmune condition where the body’s immune system attacks the insulin-producing beta cells in the pancreas.
People with Type 1 diabetes must monitor their blood sugar levels regularly. This involves pricking the finger to obtain a small blood sample, which is then tested with a glucometer. For more detailed tracking, apps like MySugr or Glucose Buddy offer convenient solutions. These apps can help log blood sugar levels, food intake, and insulin dosages, providing useful insights for overall diabetes management.
Insulin therapy is essential for individuals with Type 1 diabetes, as it replaces the missing hormone. There are various types of insulin, including rapid-acting, long-acting, and intermediate-acting forms. Understanding how these insulins work is key for proper management. Users can schedule their doses using medication management apps like Medisafe, which remind users when it’s time to take their insulin.
Education about managing Type 1 diabetes is critical. Organizations such as the Juvenile Diabetes Research Foundation (JDRF) offer resources and support. They provide information on living with diabetes, dietary guidelines, and tips for physical activity. Attending local meetings or online webinars can be beneficial for those seeking community support and knowledge.
Lastly, regular consultation with healthcare professionals is crucial. Utilizing platforms like Healthline or Diabetes.co.uk can provide updated resources and articles regarding Type 1 diabetes management. They also list features on what to discuss with a healthcare provider regarding symptoms, insulin therapy, and potential complications, ensuring comprehensive care.
Exploring Type 2 Diabetes
Type 2 diabetes is a metabolic disorder characterized by insulin resistance, where the body does not use insulin effectively. It is more prevalent than Type 1 and often develops in adults, although it is increasingly seen in children and adolescents. Lifestyle choices, including diet and physical activity, are significant factors in its onset. Understanding what contributes to Type 2 diabetes is vital for prevention and management.
Monitoring blood sugar levels is also essential for those with Type 2 diabetes. Patients can use health apps like Glucose Buddy to log their readings and track their progress over time. These platforms provide helpful graphs that allow individuals to recognize patterns in their glucose levels and make necessary adjustments.
Diet plays a crucial role in managing Type 2 diabetes. Adopting a balanced diet full of whole grains, vegetables, lean proteins, and healthy fats can help control blood sugar levels. Many apps, such as MyFitnessPal, can assist in meal planning and tracking nutritional intake. They often include large food databases to simplify counting carbohydrates and calories.
Physical activity is another key aspect of managing Type 2 diabetes. Regular exercise can increase insulin sensitivity and lower blood sugar levels. Individuals can use fitness apps like Fitbit or Google Fit to monitor their activity levels. These apps often include features that track steps, workouts, and overall wellness.
Support groups and educational programs can provide valuable resources for those living with Type 2 diabetes. Websites like Diabetes.co.uk or the American Diabetes Association offer extensive resources, including articles, forums, and tips for managing diabetes effectively. They also host community events and webinars to enhance knowledge and foster support for those affected.
Key Differences Between Type 1 and Type 2 Diabetes
Understanding the key differences between Type 1 and Type 2 diabetes is essential for individuals affected by either condition. Type 1 diabetes is an autoimmune disease that generally develops in childhood or young adulthood, while Type 2 diabetes is primarily associated with lifestyle factors and typically occurs later in life. Knowing these differences is vital for proper management and treatment strategies.
Another significant difference is the cause of each type. In Type 1 diabetes, the body’s immune system attacks insulin-producing cells in the pancreas, leading to little or no production of insulin. In contrast, Type 2 diabetes arises when cells become resistant to insulin or when the pancreas fails to produce enough insulin to maintain normal glucose levels.
Management of both types varies significantly. Type 1 diabetes requires lifelong insulin therapy. Users can benefit from apps like MySugr to help manage their dosing and track insulin usage. For Type 2 diabetes, management may include lifestyle changes such as diet and exercise, oral medications, or insulin therapy in some cases.
Blood sugar monitoring is essential for both types but may differ in frequency and methods. Individuals with Type 1 diabetes often test more frequently throughout the day. Tools such as continuous glucose monitors (CGMs) can help manage this process effectively. For Type 2, monitoring may not be as frequent and can often be managed through regular healthcare check-ups and diabetic apps.
Lastly, the long-term complications associated with both diseases can vary. While both increase the risk of similar complications like heart disease and kidney failure, Type 1 diabetes may lead to specific issues related to chronic insulin dependence. Resources from the American Diabetes Association can provide insights on maintaining overall health and managing complications for each type of diabetes.
**Understanding Type 1 Diabetes and Type 2 Diabetes**
Overview of Diabetes Types
Diabetes is a chronic condition that occurs when the body cannot effectively manage blood sugar levels. The two main types, Type 1 diabetes and Type 2 diabetes, have different causes, symptoms, and treatments. Type 1 diabetes is often diagnosed in childhood or adolescence, while Type 2 diabetes is more commonly found in adults, particularly those who are overweight or have a sedentary lifestyle. Understanding these distinctions is crucial for effective management and treatment.
Type 1 diabetes is an autoimmune condition where the body attacks insulin-producing cells in the pancreas. As a result, individuals with Type 1 diabetes must take insulin daily to manage their blood sugar levels. Type 2 diabetes, on the other hand, is often related to lifestyle factors such as diet and exercise. The body becomes resistant to insulin, or the pancreas doesn’t produce enough insulin to maintain normal blood sugar levels.
Both types of diabetes can lead to serious health complications if not managed properly, including heart disease, kidney failure, and vision loss. Awareness of the symptoms, such as frequent urination, extreme thirst, and fatigue, can aid in early detection and treatment. Management practices vary significantly between the two types, impacting the lifestyle choices individuals must make.
When discussing Type 1 diabetes and Type 2 diabetes, it’s important to consider their respective risk factors. Genetic predisposition plays a significant role in Type 1 diabetes, while Type 2 diabetes is more influenced by environmental and lifestyle factors. These insights can guide prevention strategies and inform treatment decisions for patients.
In conclusion, understanding the differences between Type 1 diabetes and Type 2 diabetes is essential for both patients and healthcare providers. Early diagnosis and appropriate management are key to maintaining health and preventing complications associated with diabetes.
**Management Strategies for Type 1 Diabetes and Type 2 Diabetes**
Effective Management Techniques
Managing diabetes effectively requires a comprehensive strategy that incorporates diet, exercise, monitoring blood sugar levels, and medication as needed. For individuals with Type 1 diabetes, this often includes taking insulin daily and being vigilant about carbohydrate intake. Conversely, those managing Type 2 diabetes may initially manage their condition through lifestyle changes alone.
When choosing a diet, it is essential to focus on balanced nutrition. A diet rich in whole grains, fruits, vegetables, and lean proteins can help regulate blood sugar levels. For those with Type 2 diabetes, losing excess weight can improve insulin sensitivity, making it easier to manage blood sugar levels.
Regular physical activity plays a critical role in diabetes management. Exercise helps improve insulin sensitivity and lowers blood sugar levels. A combination of aerobic exercise and strength training can be particularly beneficial. Individuals should aim for at least 150 minutes of moderate exercise weekly, which can be broken down into manageable sessions.
Monitoring blood sugar is a vital component of managing both types of diabetes. Individuals should follow their healthcare provider’s recommendations regarding how frequently to check their blood sugar and what targets they should aim for. This regular monitoring helps individuals understand how their food, activity, and medications affect their blood sugar levels.
Ultimately, effective diabetes management is a personalized process. Working closely with healthcare professionals to develop a tailored plan is crucial for success in managing Type 1 diabetes and Type 2 diabetes, leading to better health outcomes.
**Exploring the Link Between Type 1 Diabetes and Type 2 Diabetes**
Underlying Connections and Differences
While Type 1 diabetes and Type 2 diabetes are considered separate conditions, they share some commonalities and risk factors. Both conditions involve issues with insulin, the hormone responsible for regulating blood sugar levels. However, the mechanisms behind these issues differ considerably.
One notable connection is the impact of genetics on diabetes. Family history can play a significant role in the development of both Type 1 and Type 2 diabetes. Individuals with a family history of these conditions may be at an increased risk of developing diabetes themselves, highlighting the importance of monitoring and lifestyle choices.
Furthermore, both types of diabetes require ongoing education and awareness. Patients must stay informed about their condition, including recognizing symptoms, understanding medication, and knowing how to manage potential complications. Educational resources can empower individuals with Type 1 diabetes and Type 2 diabetes to take control of their health.
Despite these shared characteristics, the differences between Type 1 and Type 2 diabetes are pronounced. Type 1 diabetes typically presents suddenly and requires lifelong insulin therapy, while Type 2 diabetes develops gradually and may initially be managed with lifestyle modifications. Additionally, the age of onset and the prevalence of genetic factors vary between the two types.
In conclusion, understanding the link between Type 1 diabetes and Type 2 diabetes enhances our comprehension of these conditions. By recognizing both the similarities and differences, individuals can better navigate their healthcare journeys and seek appropriate support.
**Lifestyle Changes to Improve Diabetes Management**
Healthy Habits for Better Control
Embracing lifestyle changes is vital for effectively managing both Type 1 diabetes and Type 2 diabetes. Adopting healthier eating habits, engaging in regular physical activity, and maintaining a healthy weight can significantly improve blood sugar control and overall well-being.
Nutrition plays a critical role in diabetes management. Individuals should focus on consuming a diet that is low in refined sugars and high in complex carbohydrates. Incorporating foods such as whole grains, legumes, and a variety of fruits and vegetables can provide essential nutrients while helping to maintain stable blood sugar levels.
Hydration is equally important; drinking plenty of water can help the body function optimally and assist in digestion. Individuals with Type 1 diabetes and Type 2 diabetes should be mindful of their beverage choices, as sugary drinks can quickly lead to spikes in blood sugar. It’s best to choose water, herbal teas, or other low-calorie beverages.
Regular physical activity is another essential component of diabetes management. Aim for a mix of cardiovascular and strength-training exercises for optimal results. Activities like walking, cycling, swimming, or resistance training can help reduce body fat, enhance insulin sensitivity, and improve overall health.
Stress management techniques are also crucial. High-stress levels can negatively impact blood sugar management. Practices such as yoga, meditation, and deep-breathing exercises can be beneficial for reducing stress and promoting emotional well-being. By cultivating a healthy lifestyle, individuals can create a positive environment for managing Type 1 diabetes and Type 2 diabetes.
**Innovations in Diabetes Treatment and Technology**
Emerging Solutions for Diabetes Management
Advancements in technology and research have led to innovative solutions for managing diabetes. For people living with Type 1 diabetes and Type 2 diabetes, these advancements can enhance blood sugar control and improve quality of life. One of the most appealing developments is the use of continuous glucose monitors (CGMs), which provide real-time data on blood sugar levels.
CGMs can help individuals make informed decisions about their food and activity levels, allowing for more precise management of their diabetes. Additionally, insulin pumps offer a convenient way for those with Type 1 diabetes to deliver insulin continuously throughout the day, promoting better glycemic control.
Telehealth has also become an increasingly important tool in diabetes management, particularly in recent years. Patients can consult with healthcare providers remotely, receive guidance, and access educational resources without needing to visit a medical facility. This accessibility enhances patient engagement and can lead to better adherence to treatment plans.
Research into artificial pancreas systems is also underway, with some systems already available on the market. These devices automatically monitor blood sugar levels and deliver insulin as needed, minimizing the burdens of daily management for people with Type 1 diabetes. Such innovations can transform the lives of those living with diabetes.
As new treatments and technologies continue to emerge, staying informed about the latest developments is essential for individuals with Type 1 diabetes and Type 2 diabetes. These advancements offer hope for improved management and a better quality of life for those living with diabetes.
Conclusion
Understanding the intricacies of Type 1 and Type 2 diabetes is essential for effective management and treatment. Type 1 diabetes is primarily an autoimmune condition that necessitates lifelong insulin therapy, while Type 2 diabetes is linked more closely to lifestyle choices and can often be managed through a combination of exercise, diet, and medication. Both types require consistent blood sugar monitoring and awareness of symptoms to prevent complications. The differences in causes, management strategies, and complications between the two types highlight the necessity for tailored approaches to healthcare.
To successfully navigate living with diabetes, individuals are encouraged to utilize available resources, including diabetes management apps, educational programs, and professional guidance. Organizations like the Juvenile Diabetes Research Foundation (JDRF) and the American Diabetes Association offer a wealth of information and support to empower patients and their families. These tools can enhance understanding, facilitate better diet and exercise choices, and promote a proactive approach to managing diabetes.
Finally, staying informed about innovations in diabetes treatment and technology can lead to improved outcomes and quality of life for those affected by both Type 1 and Type 2 diabetes. From continuous glucose monitors to telehealth options, these advancements are revolutionizing diabetes care and offering hope for those managing the condition. By prioritizing education and adopting healthy lifestyle habits, individuals can take charge of their health, mitigate risks, and foster a supportive community that encourages open dialogue about diabetes management.
