Diabetes 2 diabetes, or type 2 diabetes, is a chronic condition marked by high blood sugar due to the body’s ineffective use of insulin, requiring lifestyle changes, regular monitoring, and medical management to minimize health risks.
Diabetes 2 diabetes affects many people, but understanding it can help you manage your condition better. Curious about how lifestyle choices impact your health? Let’s explore some effective strategies together.
What is diabetes 2 diabetes?
Diabetes 2 diabetes, often referred to as type 2 diabetes, is a chronic metabolic disorder characterized by high blood sugar levels. This occurs when the body doesn’t effectively use insulin, a hormone produced by the pancreas that regulates blood glucose. In type 2 diabetes, the body either doesn’t produce enough insulin or the cells become resistant to its effects, leading to a buildup of glucose in the bloodstream. Over time, this can damage various organs and systems in the body.
Understanding Insulin Resistance
Insulin resistance plays a key role in the development of type 2 diabetes. Normally, insulin helps transport glucose from the bloodstream into cells, where it’s used for energy. However, in insulin resistance, the cells don’t respond properly to insulin, causing glucose to remain in the blood. This triggers the pancreas to produce more insulin to compensate, but eventually, it may not be able to keep up, leading to persistently elevated blood sugar.
Risk Factors for Diabetes 2 Diabetes
Several factors can increase the risk of developing type 2 diabetes. These include:
- Family history: Having a parent or sibling with type 2 diabetes significantly increases your risk.
- Overweight or obesity: Excess weight, especially around the abdomen, is a major risk factor.
- Physical inactivity: Lack of regular exercise contributes to insulin resistance.
- Unhealthy diet: A diet high in processed foods, sugary drinks, and saturated fats can increase your risk.
- Age: The risk of type 2 diabetes increases with age, particularly after 45.
- Certain ethnicities: African Americans, Hispanic/Latino Americans, American Indians, and Asian Americans are at higher risk.
Common symptoms to watch for
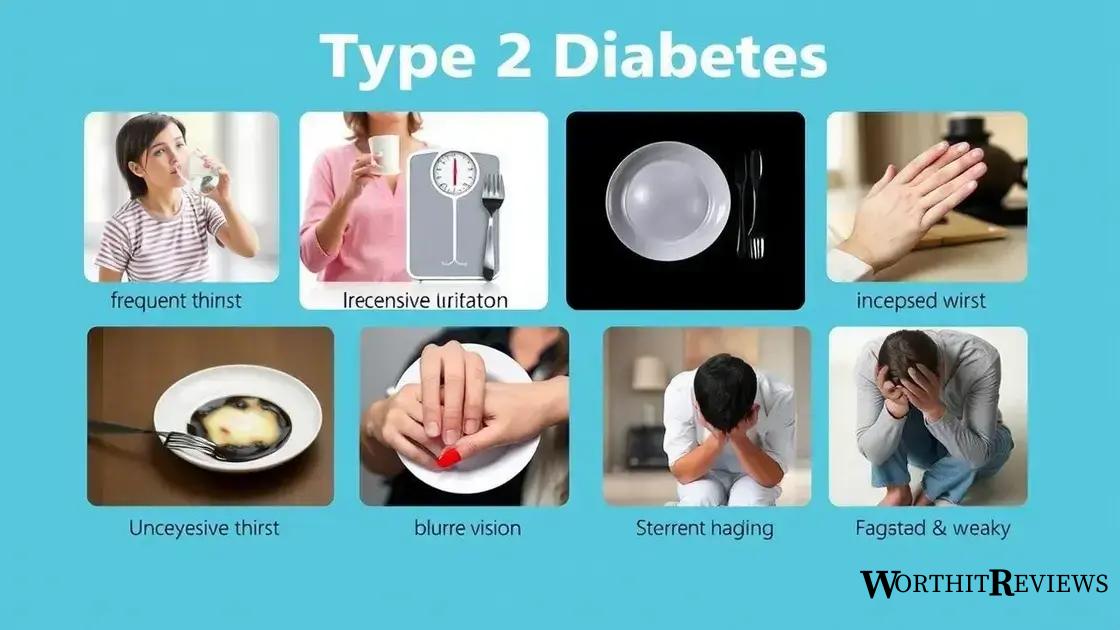
Recognizing the common symptoms of diabetes 2 diabetes is crucial for early diagnosis and management. While some individuals may experience no noticeable symptoms initially, others may develop a range of indicators that warrant medical attention. Be aware of the following:
Frequent Urination and Excessive Thirst
Increased urination (polyuria) and excessive thirst (polydipsia) are classic symptoms of diabetes. When blood sugar levels are high, the kidneys work overtime to filter and excrete the excess glucose, leading to more frequent trips to the bathroom. This fluid loss, in turn, triggers increased thirst.
Unexplained Weight Loss
In some cases, unexplained weight loss can be a sign of diabetes. When the body can’t effectively use glucose for energy, it starts breaking down muscle and fat stores for fuel, resulting in weight loss.
Increased Hunger
Despite eating, individuals with diabetes may experience persistent hunger (polyphagia). This occurs because the body’s cells aren’t receiving the glucose they need for energy, leading to a constant feeling of hunger.
Blurry Vision
High blood sugar levels can affect the lens and fluid in the eye, causing blurry vision. This symptom often improves once blood sugar levels are under control.
Slow-Healing Sores or Frequent Infections
Elevated glucose levels can impair the body’s ability to heal and fight infections, leading to slow-healing sores, frequent infections, and skin conditions like yeast infections.
Fatigue and Weakness
Fatigue and weakness are common symptoms of diabetes, often resulting from the body’s inability to properly utilize glucose for energy.
If you experience any of these symptoms, it’s important to consult a healthcare professional for proper diagnosis and guidance. Early detection and management of diabetes can help prevent serious complications.
Lifestyle changes that can make a difference
Making positive lifestyle changes plays a vital role in managing diabetes 2 diabetes and improving overall health. Even small adjustments can make a significant difference in controlling blood sugar levels, reducing the risk of complications, and enhancing quality of life. Consider incorporating the following changes:
Regular Physical Activity
Engage in regular physical activity, aiming for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, cycling, or swimming. Exercise helps improve insulin sensitivity, lower blood sugar levels, and manage weight.
Healthy Eating Habits
Adopt a balanced and nutritious diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit processed foods, sugary drinks, and saturated and unhealthy fats. A registered dietitian can help create a personalized meal plan.
Weight Management
If you’re overweight or obese, losing even a small amount of weight can significantly improve insulin sensitivity and blood sugar control. A combination of healthy eating and regular exercise is essential for effective weight management.
Stress Management
Chronic stress can elevate blood sugar levels. Practice stress-reducing techniques such as yoga, meditation, deep breathing exercises, or spending time in nature. Finding healthy ways to manage stress is crucial for diabetes management.
Quit Smoking
Smoking increases the risk of developing diabetes complications. If you smoke, quitting is one of the best things you can do for your health.
Adequate Sleep
Getting enough sleep is essential for overall health and diabetes management. Aim for 7-9 hours of quality sleep per night. Insufficient sleep can disrupt hormone balance and affect blood sugar control.
By embracing these lifestyle changes, you can gain better control over your diabetes, reduce your risk of complications, and improve your overall well-being.
Nutrition tips for managing diabetes

Proper nutrition is a cornerstone of managing diabetes 2 diabetes. Making informed food choices can help regulate blood sugar levels, maintain a healthy weight, and reduce the risk of complications. Consider these nutrition tips:
Focus on Whole, Unprocessed Foods
Prioritize whole, unprocessed foods like fruits, vegetables, whole grains, lean proteins, and healthy fats. These foods are rich in nutrients and fiber, which helps regulate blood sugar and promote satiety.
Control Carbohydrate Intake
While carbohydrates are an essential part of a healthy diet, it’s important to monitor and control your intake, especially if you have diabetes. Choose complex carbohydrates like whole grains over refined carbohydrates like white bread and sugary drinks. Work with a registered dietitian or certified diabetes educator to determine the appropriate carbohydrate intake for your individual needs. They can teach you carbohydrate counting and help you understand the glycemic index of foods.
Choose Healthy Fats
Include healthy fats in your diet, such as those found in avocados, nuts, seeds, and olive oil. Healthy fats support heart health and help you feel full, which can aid in weight management.
Limit Added Sugars
Minimize your consumption of added sugars found in sugary drinks, desserts, and processed foods. These sugars can cause spikes in blood sugar and contribute to weight gain.
Monitor Portion Sizes
Pay attention to portion sizes to avoid overeating and manage your calorie intake. Use smaller plates and measuring cups to help control portions.
Hydrate Regularly
Drink plenty of water throughout the day. Water helps flush out excess glucose and keeps you hydrated.
Meal Planning and Preparation
Plan your meals and snacks ahead of time to ensure you make healthy choices. Preparing meals at home allows you to control ingredients and portion sizes.
By following these nutrition tips and working with a healthcare professional, you can develop a personalized eating plan that supports your diabetes management goals.
The importance of regular check-ups
Regular check-ups are essential for managing diabetes 2 diabetes effectively. These visits allow healthcare professionals to monitor your condition, assess your treatment plan, and identify any potential complications early on. Here’s why regular check-ups are so important:
Monitoring Blood Sugar Levels
Regular A1C tests measure your average blood sugar levels over the past 2-3 months, providing valuable insights into your diabetes management. Your doctor may also recommend regular blood glucose monitoring at home.
Blood Pressure and Cholesterol Checks
People with diabetes are at increased risk of developing heart disease. Regular blood pressure and cholesterol checks help manage these risk factors.
Foot Exams
Diabetes can affect nerve and blood vessel health in the feet, increasing the risk of foot problems. Regular foot exams help detect and address any issues early.
Eye Exams
Diabetes can also affect eye health, potentially leading to diabetic retinopathy and vision loss. Regular eye exams with an ophthalmologist or optometrist are crucial for early detection and treatment.
Kidney Function Tests
Diabetes can damage the kidneys over time. Regular kidney function tests help monitor kidney health and detect any signs of kidney disease.
Medication Management
Regular check-ups allow your doctor to review your medications, adjust dosages as needed, and address any medication-related concerns.
Lifestyle and Self-Care Support
Your healthcare team can provide guidance and support on lifestyle changes, including diet, exercise, and stress management.
By attending regular check-ups and maintaining open communication with your healthcare team, you can proactively manage your diabetes and reduce your risk of developing serious complications.
How to cope with emotional challenges

Living with diabetes 2 diabetes can present emotional challenges. It’s important to recognize that these challenges are normal and that support is available. Consider these strategies for coping:
Acknowledge Your Feelings
Don’t dismiss or ignore your emotions. Allow yourself to feel frustration, sadness, or anger without judgment. Acknowledging your feelings is the first step towards coping effectively.
Seek Support
Connect with others who understand what you’re going through. Join a diabetes support group, talk to a therapist or counselor, or confide in trusted friends and family members. Sharing your experiences and feelings can provide comfort and reduce feelings of isolation.
Practice Self-Care
Prioritize activities that promote your physical and emotional well-being. Engage in regular exercise, get enough sleep, eat a healthy diet, and pursue hobbies and interests that bring you joy. Taking care of yourself can help you manage stress and improve your overall mood.
Focus on What You Can Control
While you can’t control having diabetes, you can control how you manage it. Focus on making healthy choices, attending regular check-ups, and following your treatment plan. Taking an active role in your diabetes management can empower you and reduce feelings of helplessness.
Seek Professional Help
If you’re struggling to cope with emotional challenges, don’t hesitate to seek professional help. A therapist or counselor can provide support and guidance in developing coping strategies.
Celebrate Small Victories
Acknowledge and celebrate your successes, no matter how small they may seem. Did you meet your exercise goal for the week? Did you make a healthy meal choice? Give yourself credit for your efforts.
Remember, you’re not alone in this journey. By utilizing these coping strategies and seeking support when needed, you can navigate the emotional challenges of diabetes and live a fulfilling life.
Managing Diabetes 2 diabetes effectively involves a multifaceted approach encompassing lifestyle adjustments, medical care, and emotional well-being. By actively participating in your care, adopting healthy habits, and seeking support when needed, you can navigate the challenges of diabetes and live a full and healthy life. Remember, knowledge is power. Understanding your condition and working closely with your healthcare team are crucial for successful diabetes management.
