Understanding the differences between type 1 and type 2 diabetes is crucial for managing these distinct conditions effectively. While both involve insulin regulation and blood sugar control, they differ significantly in their causes, symptoms, and treatment approaches.
In this article, we’ll delve into their unique characteristics, helping you distinguish between the two to empower yourself or loved ones in making informed health decisions. Whether you’re newly diagnosed or seeking clarity, this guide is here to enhance your knowledge.
Understanding Type 1 Diabetes and Its Unique Features
Type 1 diabetes is a chronic condition characterized by the body’s inability to produce insulin due to autoimmune destruction of the insulin-producing beta cells in the pancreas. This type typically occurs in children and young adults, though it can develop at any age. Recognizing its symptoms early, such as increased thirst and frequent urination, is crucial for management.
To manage Type 1 diabetes, individuals often use continuous glucose monitors (CGMs) to track their blood sugar levels. One recommended app for this is mySugr, which allows users to input their data and receive insights about their glucose levels. You can download the app on iOS and Android, which provides a user-friendly interface.
Insulin therapy is a fundamental component of managing Type 1 diabetes. This involves administering insulin through injections or an insulin pump. For an ideal dosage, patients should consult with their healthcare providers and perhaps utilize the Diabetes: Type 1 app, which helps in calculating the required insulin based on carbohydrate intake and current blood glucose levels.
Education plays a vital role in living with Type 1 diabetes. Numerous resources, such as the JDRF website, offer valuable information tailored for those diagnosed. Patients can enroll in diabetes education programs accessed through local clinics or health organizations. Using sites like https://worthitreviews.com/ can help locate credible educational materials.
Support networks, both online and offline, provide emotional and practical assistance to individuals with Type 1 diabetes. Forums such as Diabetes Daily and platforms like the ADA’s community section create space for sharing experiences and strategies for managing this condition. Engaging with peers can help foster a sense of belonging and provide tips that simplify daily diabetes management.
Exploring Type 2 Diabetes and Its Key Characteristics
Type 2 diabetes is often associated with insulin resistance, where the body does not use insulin effectively. It commonly occurs in adults, although rising obesity rates have led to more cases in younger individuals. Recognizing risk factors, such as a sedentary lifestyle and family history, is one of the first steps in prevention and management.
Management of Type 2 diabetes primarily focuses on lifestyle changes and monitoring blood sugar levels. A practical step is utilizing the Glucose Buddy app, which helps users log their meals and track their glucose levels effortlessly. By engaging with the app, individuals can identify food triggers and adjust their diets accordingly.
Nutrition plays a crucial role in managing Type 2 diabetes. Incorporating a balanced diet rich in whole foods can aid in controlling blood sugar levels. Resources like the USDA’s MyPlate website provide personalized dietary guidelines and meal-planning tips. Users can create a plan that best fits their health needs and goals.
Physical activity is another key trait in managing Type 2 diabetes effectively. Engaging in regular exercise helps increase insulin sensitivity. The Fitbit app recommends daily step goals and allows users to track their physical activities. This makes it easier to maintain an active lifestyle and keep blood sugar in check.
Regular consultations with healthcare professionals ensure that individuals with Type 2 diabetes stay informed about their condition. Utilizing platforms like Healthgrades to find local healthcare providers is essential. Regular check-ups facilitate timely adjustments to treatment plans, ensuring optimal management of the condition.
Comparing Type 1 and Type 2 Diabetes for Better Awareness
Understanding the key differences between Type 1 and Type 2 diabetes is crucial for effective awareness and management. Type 1 diabetes, often diagnosed in childhood, is an autoimmune condition where insulin production ceases. In comparison, Type 2 diabetes primarily arises due to insulin resistance and more commonly develops in adulthood.
When considering treatment options, Type 1 diabetes requires lifelong insulin therapy, as the body produces little to no insulin. For Type 2 diabetes, lifestyle changes, such as diet and exercise, are often the first line of defense, along with medications that may or may not include insulin over time. Recognizing these contrasting treatment methods can guide individuals toward effective self-management.
Prevention strategies also differ significantly between the two types. Type 1 diabetes currently has no known preventive measures due to its autoimmune nature. In contrast, Type 2 diabetes can often be prevented or delayed through a healthy lifestyle. The CDC’s Diabetes Prevention Program provides resources and support to help individuals at risk make necessary changes.
Monitoring blood glucose levels is essential for both types of diabetes, but methods may vary. Individuals with Type 1 diabetes often rely on CGMs, while those with Type 2 may use periodically glucose monitoring tools. Apps like MySugr can be beneficial for both groups, offering tracking features and personalized insights.
Lastly, emotional support plays a significant role in managing both types of diabetes. Joining community forums or local support groups fosters a sense of connection. Resources such as DiabetesSisters provide structured support tailored to the unique experiences of women with diabetes, which can be instrumental in finding camaraderie and advice.

Understanding Type 1 Diabetes and Type 2 Diabetes
Type 1 diabetes and type 2 diabetes are two distinct forms of diabetes that affect how our bodies utilize glucose, a crucial source of energy. Understanding the differences, causes, and management strategies for these conditions is vital for those diagnosed or at risk. Type 1 diabetes is a chronic condition that typically appears in childhood or adolescence, while type 2 diabetes is more prevalent in adults, often linked to obesity and physical inactivity.
Both types of diabetes share common symptoms including increased thirst, frequent urination, and fatigue. However, the underlying causes are different. Type 1 diabetes occurs when the immune system mistakenly attacks insulin-producing beta cells in the pancreas, leading to little or no insulin production. Conversely, type 2 diabetes begins with insulin resistance, where the body cannot effectively use insulin, eventually requiring the pancreas to produce more insulin.
Diagnosis for both conditions generally involves blood tests to measure glucose levels. An A1C test, for instance, reflects average blood glucose over the previous three months. Early detection and management of type 1 and type 2 diabetes are crucial to prevent further complications, such as cardiovascular disease, nerve damage, and kidney failure.
Management strategies differ significantly between the two. For type 1 diabetes, patients typically need insulin therapy from the onset, whereas type 2 diabetes management usually starts with lifestyle changes—diet and exercise—before progressing to oral medications or insulin if necessary. Regular monitoring of blood sugar levels is essential for both types, allowing individuals to make informed choices about their dietary and lifestyle habits.
Understanding these differences is important for tailoring management strategies, education, and support needed for individuals coping with either type of diabetes. There are various resources available to help patients, including diabetes education programs and support groups, which can be incredibly beneficial for those looking to lead a healthy lifestyle.
Symptoms of Type 1 Diabetes and Type 2 Diabetes
Recognizing the symptoms of type 1 diabetes and type 2 diabetes is crucial for timely diagnosis and prevention of complications. Both types share many symptoms, but their onset and additional signs may vary. Type 1 diabetes symptoms often develop suddenly and can be severe. Common symptoms include extreme thirst, frequent urination, fatigue, and blurred vision.
Individuals with type 2 diabetes might experience similar symptoms, although they often develop gradually. Many individuals may not even realize they have type 2 diabetes until complications arise. Other symptoms can include increased hunger, weight loss, tingling in hands or feet, and slow-healing sores. It’s important for anyone exhibiting these signs to seek medical attention, particularly if they have family history of diabetes.
In children and adolescents, sudden weight loss and frequent infections can also be indicators of type 1 diabetes, caused by the body’s inability to utilize glucose effectively. On the other hand, type 2 diabetes can be associated with obesity or being overweight, especially in adults. This makes lifestyle management a key factor for also preventing further complications for those diagnosed with type 2.
Regular screenings and check-ups play an essential role in early detection of symptoms. For those with high-risk factors, such as obesity, sedentary lifestyle, or family history, routine blood glucose monitoring can help in catching these symptoms before they escalate.
Being aware of these symptoms allows patients and healthcare providers to collaboratively create individualized management plans and ultimately leads to better health outcomes for individuals diagnosed with type 1 and type 2 diabetes.
Management Strategies for Type 1 Diabetes and Type 2 Diabetes
Managing type 1 diabetes and type 2 diabetes involves a comprehensive approach tailored to individual needs. For type 1 diabetes, the cornerstone of management is insulin therapy, as these patients are unable to produce insulin. Patients often adopt multiple daily injections or continuous insulin infusion via a pump. Regular monitoring of blood glucose levels is also critical to avoid hypoglycemia and maintain ideal glucose levels.
In contrast, management plans for type 2 diabetes typically start with lifestyle changes. Regular physical activity and a balanced diet are essential components. Patients are encouraged to engage in at least 150 minutes of moderate exercise per week, along with dietary adjustments emphasizing whole foods, fruits, vegetables, lean proteins, and whole grains while minimizing processed foods.
If lifestyle modifications are insufficient to control blood glucose levels, medications may be introduced. Oral medications like Metformin can help improve insulin sensitivity and lower blood sugar. In some cases, insulin therapy may also be necessary for type 2 diabetes patients who can no longer maintain glycemic control.
Additionally, regular follow-ups with healthcare providers are important for monitoring progress and adjusting treatment plans as necessary. A diabetes care team may include doctors, certified diabetes educators, and dietitians to provide comprehensive support.
Staying informed about diabetes management, utilizing technology such as continuous glucose monitors, and participating in support groups can significantly enhance self-management skills. Empowering patients with knowledge fosters a more proactive approach to living with type 1 diabetes and type 2 diabetes.
The Role of Diet in Type 1 Diabetes and Type 2 Diabetes Management
Diet plays a crucial role in managing both type 1 diabetes and type 2 diabetes, influencing blood glucose levels and overall health. For those with type 1 diabetes, coordinates with insulin therapy is essential to maintain stable blood sugar levels. A balanced diet that emphasizes carbohydrates counting can significantly reduce the risk of hypoglycemia or hyperglycemia. Foods high in fiber, such as whole grains, vegetables, and fruits, should be prioritized as they help regulate blood glucose levels.
In type 2 diabetes, diet becomes an even more critical part of management, as it can significantly impact insulin sensitivity and weight control. Patients are often advised to adopt a Mediterranean-style diet, rich in healthy fats (like olive oil), whole grains, lean proteins, and plenty of fruits and vegetables. This not only helps in stabilizing blood sugar levels but also contributes to weight loss, which is beneficial for overall health.
Monitoring portion sizes is equally important for both types. Individuals with diabetes need to be mindful of how much they eat to prevent spikes in blood sugar levels. Implementing tools such as portion plates or measuring cups can aide in accurate portion control.
Alcohol consumption should also be approached cautiously, as it can interfere with glucose levels and the overall management plan. Educating oneself on the glycemic index of various foods can further assist individuals in making informed dietary choices.
Seeking the guidance of a registered dietitian specialized in diabetes can provide tailored dietary advice, ensuring individuals meet their nutritional needs while effectively managing their diabetes. This integrated approach to a healthy diet can enhance the overall well-being of individuals with type 1 diabetes and type 2 diabetes.
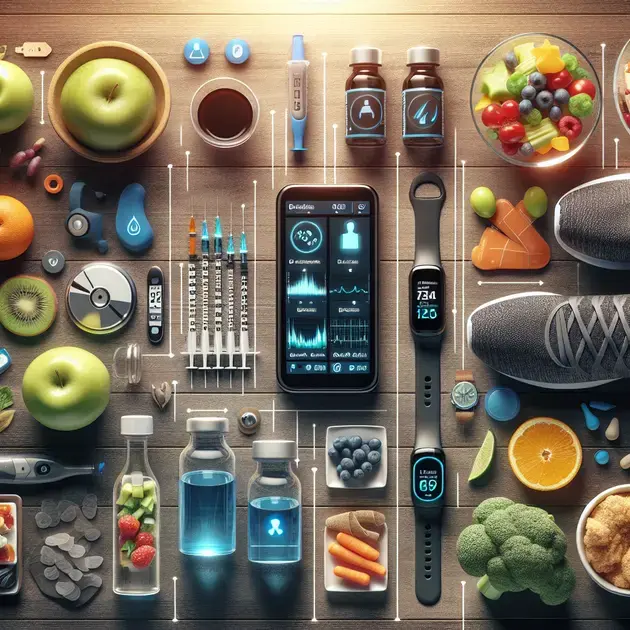
Technological Advances in Diabetes Management for Type 1 and Type 2 Types
Advancements in technology are transforming the management of type 1 diabetes and type 2 diabetes, making it easier for individuals to control their blood glucose levels effectively. One of the most significant improvements is the development of continuous glucose monitoring (CGM) systems. These devices provide real-time glucose readings and trends, allowing users to adjust their insulin intake or dietary choices swiftly.
Insulin pumps have also revolutionized type 1 diabetes management, offering a more flexible approach to insulin delivery. These devices can be programmed to deliver precise amounts of insulin throughout the day, closely mimicking the body’s natural functions. With the integration of smart technology, patients can monitor their glucose levels, receive alerts for high or low readings, and manage their diabetes through mobile applications.
For individuals with type 2 diabetes, technological innovations include digital health solutions and wearable devices that promote active living and better dietary choices. Fitness trackers, for instance, help individuals stay accountable for their exercise routines and connect with supportive online communities for motivation.
Telehealth has also gained prominence, particularly during recent global health crises. Patients can consult their healthcare providers remotely, enabling easier access to professional guidance without travel concerns. This convenience is vital for maintaining consistent diabetes management and support.
As technology continues to evolve, the future of diabetes management looks promising. From automated insulin delivery systems to enhanced educational tools, these advancements greatly improve the quality of life for individuals managing type 1 diabetes and type 2 diabetes. Staying informed and adapting to these new technologies can lead to more successful diabetes outcomes.
Conclusion
Understanding both Type 1 and Type 2 diabetes is essential for effective management and the overall well-being of individuals affected by these chronic conditions. Type 1 diabetes occurs predominantly in youth and necessitates lifelong insulin therapy due to the autoimmune destruction of insulin-producing cells in the pancreas. On the other hand, Type 2 diabetes is more prevalent in adults and is often linked to lifestyle factors such as diet and physical activity. Recognizing the symptoms, early diagnosis, and tailored management strategies can significantly impact the quality of life for those living with diabetes.
Management for Type 1 diabetes revolves around insulin therapy, continuous glucose monitoring, and strong educational support from healthcare providers and resources. Utilizing tools like mobile apps can help patients track their glucose levels and stay informed. In contrast, Type 2 diabetes management usually starts with lifestyle modifications focused on diet and exercise. With support from digital health solutions and healthcare professionals, individuals can implement effective strategies to lower their risk of complications.
Ultimately, the differences between Type 1 and Type 2 diabetes underscore the need for personalized approaches to diabetes management. Education, community support, and technological advancements play vital roles in empowering patients to take control of their health. By staying informed about their condition and utilizing available resources, individuals can navigate the challenges posed by diabetes, leading to healthier and more fulfilling lives. Through awareness and proactive strategies, both types of diabetes can be managed effectively, fostering a sense of community and support among those affected.
