Type 2 diabetes management involves monitoring blood sugar levels, making healthy dietary choices, exercising regularly, and possibly using medications, all while empowering yourself with knowledge and support from healthcare professionals.
Type 2 diabetes and blood sugar levels go hand in hand, affecting millions globally. Have you ever wondered how small lifestyle changes can make a big difference?
Understanding type 2 diabetes
Understanding type 2 diabetes is essential for managing your health effectively. Type 2 diabetes occurs when the body either resists the effects of insulin or doesn’t produce enough insulin to maintain normal glucose levels. This leads to higher levels of sugar in the blood.
Insulin is a hormone that helps sugar from the food you eat get into your cells to be used for energy. When insulin is not effective, the sugar stays in the bloodstream, leading to various health issues.
Some key risk factors include:
- Being overweight or obese
- Age (over 45 years)
- Family history of diabetes
- Lack of physical activity
Many people may have type 2 diabetes without knowing it, which is why regular check-ups are crucial. In fact, early detection can greatly improve management and reduce the risk of serious complications.
Common symptoms of type 2 diabetes include:
- Increased thirst
- Frequent urination
- Extreme fatigue
- Blurred vision
Understanding your body’s signals and recognizing these symptoms are all part of taking control of your health.
By learning about this condition, you can cultivate better habits that support your well-being.
The role of blood sugar levels

The role of blood sugar levels is vital in understanding type 2 diabetes and overall health. Blood sugar, or glucose, is what our bodies use for energy. After eating, your body breaks down food into glucose, which enters the bloodstream. The regulation of this glucose is crucial.
Insulin, produced by the pancreas, helps keep blood sugar levels within a normal range. When you have type 2 diabetes, this process doesn’t work effectively, leading to higher than normal blood sugar levels.
Maintaining balanced blood sugar levels is important because:
- They help prevent serious complications such as heart disease and nerve damage.
- Stable blood sugar levels support energy levels and prevent fatigue.
- They reduce the risk of hypoglycemia, a condition where blood sugar drops too low.
Monitoring your blood sugar levels regularly can provide valuable insight into how your body responds to different foods and activities. This way, you can make informed decisions about diet and exercise.
Some factors that influence blood sugar levels include:
- Food choices: Carbohydrates, in particular, have the most significant impact on glucose spikes.
- Physical activity: Exercise helps the body use glucose more efficiently.
- Stress and illness: These can cause temporary changes in blood sugar levels.
Understanding these factors will empower you to take control of your health.
Symptoms of high blood sugar
Symptoms of high blood sugar are important signs that can indicate poor blood sugar management in individuals with type 2 diabetes. Recognizing these symptoms early can help in taking timely action.
Some common symptoms include:
- Increased thirst: When blood sugar levels rise, it can lead to dehydration, causing you to feel thirsty frequently.
- Frequent urination: High blood sugar causes your kidneys to work harder to filter and absorb the excess glucose, leading to more frequent trips to the bathroom.
- Extreme fatigue: When your body can’t use glucose effectively for energy, you may feel unusually tired.
- Blurred vision: High levels of sugar can cause fluid to be pulled from the lenses of your eyes, leading to temporary vision issues.
- Slow healing: High blood sugar can affect your circulation, making it harder for cuts and bruises to heal.
It is essential to monitor these symptoms and consult a healthcare provider if you experience them. Early detection and effective management strategies can significantly improve your quality of life.
In some cases, severe symptoms can occur, like:
- Rapid weight loss
- Nausea and vomiting
- Fruity-smelling breath
- Difficulty breathing
If you experience severe symptoms, it is crucial to seek medical help immediately.
Dietary changes for blood sugar control

Dietary changes for blood sugar control are essential for managing type 2 diabetes effectively. By making smart food choices, you can help stabilize your blood sugar levels. Here are some key strategies:
Choose whole foods: Incorporating whole grains, vegetables, fruits, and lean proteins into your diet is beneficial. Whole foods are typically lower in sugar and higher in fiber, which slows the absorption of glucose.
Monitor carbohydrate intake: Carbohydrates directly affect blood sugar levels. Understanding how much and what type of carbohydrates you are consuming is crucial. Opt for complex carbs like brown rice and whole grain bread, which digest more slowly.
Control portion sizes: Eating smaller, balanced meals throughout the day can help prevent spikes in blood sugar. Use measuring cups or a food scale to keep portions in check.
Include healthy fats: Healthy fats such as avocados, nuts, and olive oil can improve heart health and help you feel full. This can prevent overeating and make it easier to maintain stable blood sugar levels.
Stay hydrated: Drinking enough water is vital. It helps your kidneys flush out excess sugar through urine. Aim for at least 8 cups of water a day.
Limit processed foods: Processed foods often contain added sugars and unhealthy fats that can interfere with blood sugar control. Focus on fresh, unprocessed ingredients instead.
Making these dietary changes may not only help in managing blood sugar but can also lead to overall improved health and well-being.
Exercise and its impact on blood sugar
Exercise and its impact on blood sugar is a crucial topic for individuals with type 2 diabetes. Regular physical activity can significantly help in managing blood sugar levels. Here’s how exercise benefits your body:
Increased insulin sensitivity: Exercise improves how your body uses insulin. When you exercise, your muscles take up more glucose, which helps lower blood sugar levels.
Weight management: Physical activity helps in maintaining a healthy weight. Losing weight can improve blood sugar control and reduce the risk of complications.
Lower blood sugar spikes: Engaging in aerobic activities such as walking, swimming, or cycling can prevent blood sugar spikes after meals. This is particularly useful for those who struggle with post-meal hyperglycemia.
Stress reduction: Exercise is an effective way to reduce stress, which can impact blood sugar levels. Activities like yoga or tai chi not only promote physical health but also help in maintaining emotional well-being.
Recommendations for exercise: Aim for at least 150 minutes of moderate-intensity aerobic activity each week. Additionally, incorporating strength training exercises on two or more days a week can further enhance blood sugar management.
Always consult a healthcare provider before starting a new exercise routine, especially if you have existing health conditions. They can help tailor a program that suits your individual needs and fitness levels.
Monitoring blood sugar levels effectively
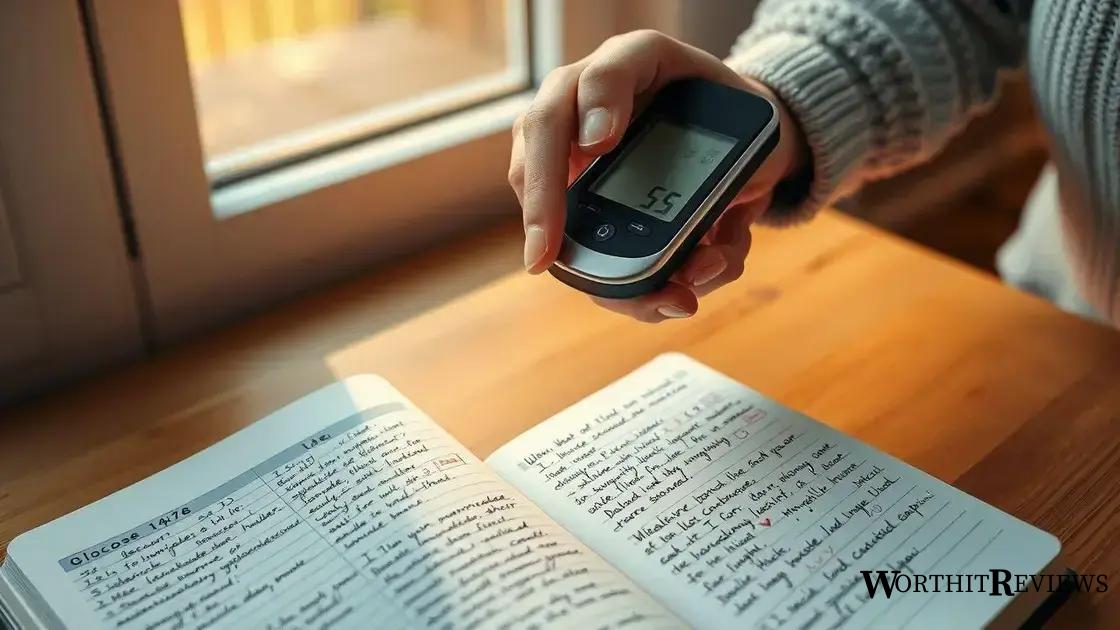
Monitoring blood sugar levels effectively is crucial for managing type 2 diabetes. Regular checks can help you understand how food, activity, and medication affect your glucose levels. Here are key points to consider:
Understanding monitoring tools: There are various devices available for monitoring blood sugar, including traditional glucose meters and continuous glucose monitors (CGMs). Each has its own benefits, so choose one that fits your lifestyle.
Recommended monitoring frequency: Many people with diabetes are advised to check their blood sugar levels at least once a day, but this can vary based on individual needs. Your healthcare provider can help determine the right schedule.
Timing matters: It’s important to know when to check your blood sugar. Common times include before meals, two hours after eating, and before bed. These checks can help you see patterns in how your body responds to food and activities.
Keeping a log: Record your blood sugar readings, along with notes about meals, exercise, and medications. This log can help you and your healthcare team identify patterns and make informed adjustments.
Interpreting the results: Understand what your blood sugar numbers mean. Target ranges can differ for individuals, but generally, fasting blood sugar should be between 70-130 mg/dL. Knowing these ranges can aid in effective management.
Responding to high or low levels: Have a plan in place for what to do if your blood sugar is too high or too low. This may include dietary adjustments, exercise, or medication changes.
Medications for type 2 diabetes
Medications for type 2 diabetes play an essential role in managing blood sugar levels when lifestyle changes alone aren’t enough. There are several types of medications available, and your healthcare provider can help determine which one is best for you.
Metformin: This is often the first medication prescribed for type 2 diabetes. Metformin helps reduce glucose production in the liver and improves insulin sensitivity, making it easier for your body to use sugar.
Sulfonylureas: These medications stimulate the pancreas to produce more insulin. Common examples include glipizide and glimepiride. They can be effective but may lead to low blood sugar if not managed carefully.
GLP-1 receptor agonists: These drugs mimic the effects of the hormones that increase insulin secretion. They also help slow gastric emptying, which can reduce cravings. Examples include liraglutide and semaglutide. They may also assist with weight loss.
SGLT2 inhibitors: Medications such as canagliflozin and empagliflozin help your kidneys remove excess sugar from the blood through urine. They can provide a dual benefit by also lowering the risk of heart disease.
Insulin therapy: Some individuals with type 2 diabetes may eventually need insulin injections. Insulin helps lower blood glucose levels by facilitating the entry of sugar into the cells for energy.
It’s crucial to take medications as prescribed and maintain regular communication with your healthcare provider to manage your condition effectively. Monitoring your blood sugar levels will indicate how well your medication regimen is working.
Empowering yourself with knowledge

Empowering yourself with knowledge is essential for effectively managing type 2 diabetes. Education about your condition not only boosts your confidence but also enables you to make informed decisions regarding your health.
Understanding diabetes: Start by learning how type 2 diabetes affects your body. Knowing the role of insulin and how blood sugar levels impact your health will provide a solid foundation for management strategies.
Staying informed: Utilize reliable resources such as diabetes education programs, books, and websites from reputable organizations. Regularly updating your knowledge can help you stay abreast of new treatments and management techniques.
Joining support groups: Connecting with others facing similar challenges can be motivating. Support groups offer a sense of community where you can share experiences, tips, and encouragement.
Monitoring your condition: Keep track of your blood sugar levels, diet, and medications. Understanding your personal data provides valuable insights into what works for you, allowing for better adjustments.
Engaging with healthcare professionals: Don’t hesitate to ask questions during doctor’s visits. Your healthcare team can provide tailored advice and tips, making it essential to communicate openly about your experiences and concerns.
Knowledge is power. The more you understand about your health, the more control you have over managing your diabetes effectively.
In summary, taking control of type 2 diabetes
Managing type 2 diabetes involves understanding your body and making informed decisions about your health. With the right knowledge, you can effectively monitor your blood sugar levels, make healthy dietary choices, and engage in regular exercise.
Medications play a crucial role in blood sugar management, but they work best when combined with a healthy lifestyle. Staying informed and seeking support from healthcare professionals and community groups can empower you to navigate your condition with confidence.
Remember, empowering yourself with knowledge is the first step toward better health. Take charge of your diabetes journey and embrace the positive changes that come with it.
