Type 1 diabetes results from the immune system attacking insulin-producing cells, while type 2 diabetes is often linked to lifestyle factors, and both types require distinct management strategies to control blood sugar levels effectively.
Type 2 diabetes and type 1 diabetes might sound similar, but these conditions impact lives in distinct ways. Have you ever wondered how lifestyle factors influence type 2 compared to type 1? Let’s dive in.
What are the main differences between type 1 and type 2 diabetes?
Understanding the differences between type 1 diabetes and type 2 diabetes is crucial for managing these conditions effectively. While both types involve issues with insulin, they have distinct characteristics and causes.
Type 1 Diabetes
Type 1 diabetes is an autoimmune condition where the immune system attacks insulin-producing cells in the pancreas. This usually occurs in children and young adults, but it can develop at any age. Individuals with type 1 diabetes must take insulin daily to survive.
Type 2 Diabetes
Type 2 diabetes, on the other hand, typically develops in adults and is often linked to lifestyle factors such as obesity and lack of physical activity. In this type, the body either becomes resistant to insulin or doesn’t produce enough insulin. Lifestyle changes, medication, and, in some cases, insulin therapy are commonly used to manage type 2 diabetes.
Symptoms
The symptoms of both conditions can overlap, but some differences exist. Common symptoms include increased thirst, frequent urination, and fatigue. However, type 1 diabetes symptoms tend to develop rapidly, while type 2 symptoms may appear gradually over time.
Long-Term Health Effects
The long-term effects of both types can be serious if not managed properly. Type 1 diabetes can lead to complications such as heart disease, kidney damage, and nerve issues. Type 2 diabetes also poses similar risks but may additionally lead to complications related to obesity and metabolism.
Causes of type 1 diabetes versus type 2 diabetes
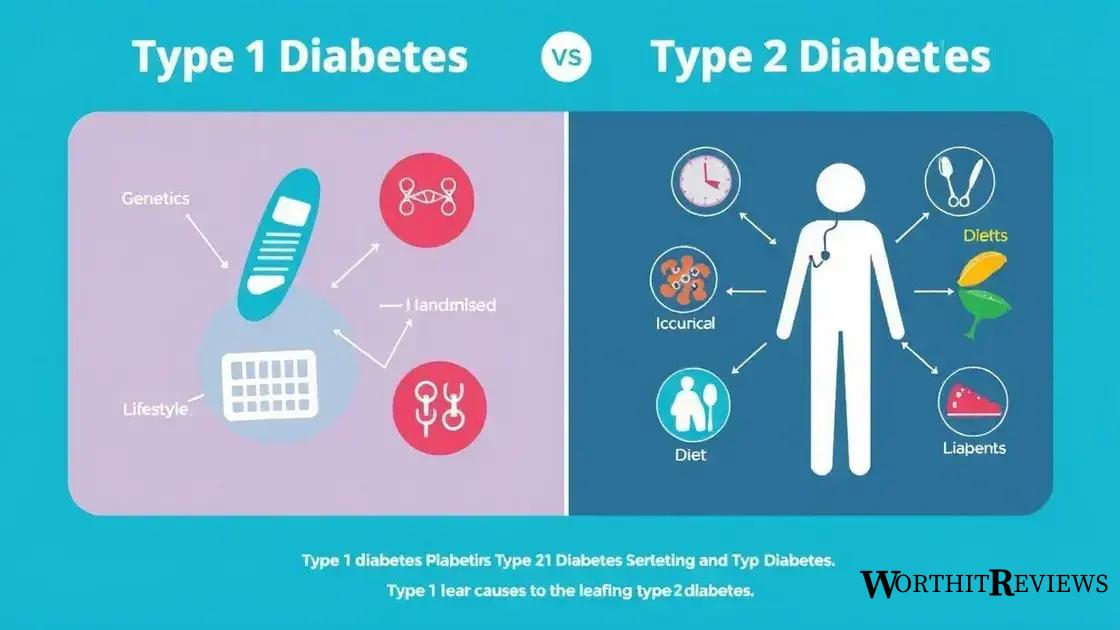
The causes of type 1 diabetes and type 2 diabetes differ significantly, impacting how each type is approached in terms of treatment and management.
Causes of Type 1 Diabetes
Type 1 diabetes is primarily caused by an autoimmune response. In this case, the body mistakenly attacks and destroys the insulin-producing cells in the pancreas. This type is not linked to lifestyle factors. Genetics may play a role, as having a family history of type 1 diabetes can increase the risk.
Causes of Type 2 Diabetes
Type 2 diabetes is largely influenced by lifestyle factors and genetics. Common causes include:
- Obesity: Excess body weight can lead to insulin resistance.
- Lack of Physical Activity: A sedentary lifestyle contributes to weight gain and impacts insulin sensitivity.
- Unhealthy Diet: Diets high in refined sugars and processed foods can increase the risk.
- Age: While type 2 diabetes can occur at any age, the risk increases as people grow older.
Several studies have shown that lifestyle changes can significantly reduce the risk of developing type 2 diabetes, showcasing the importance of healthy living.
Symptoms: How they manifest differently in type 1 and type 2
The symptoms of type 1 diabetes and type 2 diabetes can appear similar, but they manifest differently in many cases. Recognizing these differences is key to understanding and managing each type effectively.
Symptoms of Type 1 Diabetes
Symptoms of type 1 diabetes often emerge suddenly. Individuals may experience:
- Increased Thirst: A common complaint as the body tries to cope with high blood sugar levels.
- Frequent Urination: The kidneys work overtime to eliminate excess glucose through urine.
- Extreme Hunger: Despite eating, the body cannot properly use glucose, leading to feelings of hunger.
- Unintentional Weight Loss: The body starts to use muscle and fat for energy when it lacks insulin.
- Fatigue: Without enough insulin, energy levels drop significantly.
Symptoms of Type 2 Diabetes
In contrast, symptoms for type 2 diabetes usually develop gradually and may include:
- Increased Thirst and Frequent Urination: Similar to type 1 diabetes, but these symptoms may be less noticeable at first.
- Blurred Vision: High blood sugar levels can affect eye lenses, leading to vision problems.
- Slow Healing of Cuts and Bruises: The body’s ability to heal is impaired.
- Areas of Darkened Skin: Often seen in armpits or neck, indicating insulin resistance.
- Tingling or Numbness: Resulting from nerve damage due to high blood sugar levels.
Overall, while both types share some symptoms, individuals with type 1 diabetes often experience quicker and more severe symptoms compared to those with type 2 diabetes.
Management strategies for type 1 and type 2 diabetes
Managing type 1 diabetes and type 2 diabetes effectively requires different strategies, as each condition has unique challenges. Here are key management strategies for each type.
Management Strategies for Type 1 Diabetes
Individuals with type 1 diabetes need to follow a structured management plan that includes:
- Insulin Therapy: Mandatory for survival, insulin must be administered through injections or an insulin pump to maintain blood glucose levels.
- Monitoring Blood Sugar: Regularly checking blood glucose levels helps adjust insulin doses and understand how food, exercise, and stress affect these levels.
- Healthy Eating: A balanced diet with appropriate carbohydrates is essential. Carbohydrate counting can help manage blood sugar spikes.
- Regular Exercise: Physical activity is vital for overall health and can help regulate blood sugar levels. However, it should be balanced with insulin and food intake.
- Education and Support: Knowledge about diabetes management, including how to handle emergency situations, is crucial.
Management Strategies for Type 2 Diabetes
For type 2 diabetes, management focuses on lifestyle changes along with medication if necessary:
- Diet Modification: Incorporating more whole foods, such as fruits, vegetables, and whole grains, while reducing sugar and processed foods.
- Physical Activity: Aim for at least 150 minutes of moderate aerobic activity per week, like walking or cycling, to improve insulin sensitivity.
- Weight Management: Losing even a small percentage of body weight can significantly improve blood sugar control and potentially reverse type 2 diabetes.
- Medication: Depending on individual needs, medications such as metformin may be prescribed to help control blood sugar levels.
- Regular Health Check-Ups: Monitoring for complications, including heart disease, kidney function, and eye health, is essential for long-term management.
Both types of diabetes require a comprehensive approach that includes education, lifestyle changes, and regular monitoring.
Risks associated with both types of diabetes
Both type 1 diabetes and type 2 diabetes come with their own sets of risks and complications that can impact long-term health. Understanding these risks is crucial for effective management.
Risks Associated with Type 1 Diabetes
Individuals with type 1 diabetes face several risks, including:
- Diabetic Ketoacidosis (DKA): A serious condition that arises when the body produces high levels of ketones due to insufficient insulin.
- Hypoglycemia: Low blood sugar can happen from too much insulin or inadequate food intake, leading to symptoms like dizziness and confusion.
- Long-Term Complications: Chronic high blood sugar levels can cause damage to vital organs, leading to heart disease, kidney failure, and nerve damage.
Risks Associated with Type 2 Diabetes
Type 2 diabetes also presents significant risks, such as:
- Cardiovascular Disease: People with type 2 diabetes are at an increased risk for heart attacks and strokes due to the effects of high blood sugar on blood vessels.
- Neuropathy: High blood sugar can damage nerves, especially in the extremities, leading to pain, tingling, or loss of sensation.
- Eye Complications: Conditions like diabetic retinopathy can lead to vision loss if blood sugar levels remain uncontrolled.
- Kidney Disease: Over time, diabetes can harm the kidneys’ filtering system, potentially resulting in kidney failure.
Both types of diabetes require consistent monitoring and management to minimize these risks and maintain overall health.
Living with diabetes: Stories from individuals
Living with diabetes can vary greatly from person to person. Here are a few stories that highlight different experiences and strategies from individuals managing both type 1 diabetes and type 2 diabetes.
Story of a Type 1 Diabetes Patient
Maria was diagnosed with type 1 diabetes at age 12. Dealing with daily insulin injections was challenging, especially as a teenager. She learned to monitor her blood sugar closely and found that keeping a food diary helped her understand how different foods affected her. She also joined a support group, which provided her with the emotional strength to cope with her condition.
Story of a Type 2 Diabetes Patient
John was diagnosed with type 2 diabetes in his late 40s. At first, he felt overwhelmed and confused about how to manage his health. He started by making simple changes, such as adding more vegetables to his meals and taking daily walks. Over time, these small changes led to significant weight loss and improved blood sugar control. John enjoys sharing his journey on social media to inspire others facing similar challenges.
Living with Both Types
Sara, a 30-year-old nurse, juggles work and managing her type 1 diabetes. Her experience taught her the importance of being organized with her medications and meal planning. She emphasizes the need for education and awareness, explaining how staying informed about diabetes advancements has helped her live a healthier life. Sara also speaks about the significance of resilience and having a supportive community.
Each person’s journey with diabetes is unique. Some face immediate challenges like learning to use insulin pumps, while others might manage their diabetes through lifestyle changes. Sharing these experiences fosters understanding and encourages others to seek support and guidance in their own journeys.
Understanding and Managing Diabetes
Living with diabetes, whether type 1 or type 2, requires knowledge and commitment. Each person’s experience is unique, with different challenges and strategies for management.
Through stories shared by individuals, we see how critical it is to stay informed, seek support, and make lifestyle changes. From implementing insulin therapy to adjusting diets and engaging in regular physical activity, there are many ways to manage diabetes effectively.
Moreover, understanding the risks associated with both types can empower individuals to take proactive steps to protect their health. As we share these insights and personal journeys, we hope to inspire others facing diabetes to engage in their care actively.
Ultimately, with the right support and resources, people with diabetes can lead full and healthy lives.
